
 July 26, 2022 | 3 minutes read time
July 26, 2022 | 3 minutes read timeThe most amazing invention in the field of Cardiology has been the implantable pacemaker in the year 1958. The implantation technique has evolved a lot since the first implantation. Several innovations have been undertaken to improve the effectiveness, battery life of the implant and patient outcomes. The complication rate however minimal, is there with the transvenous technique e.g. pneumothorax, infection, pocket hematoma, subclavian venous thrombosis, lead fractures and insulation break.
To sum up, the pacemaker implantation technique is an art that has a lot of room for improvement and refinement. A new implantation technique to improve the procedure and possibly reduce the rate of complication markedly came to existence in form of Leadless Pacemaker in year 2016. The goal of the leadless pacemaker was to eliminate lead related and pocket related complications.
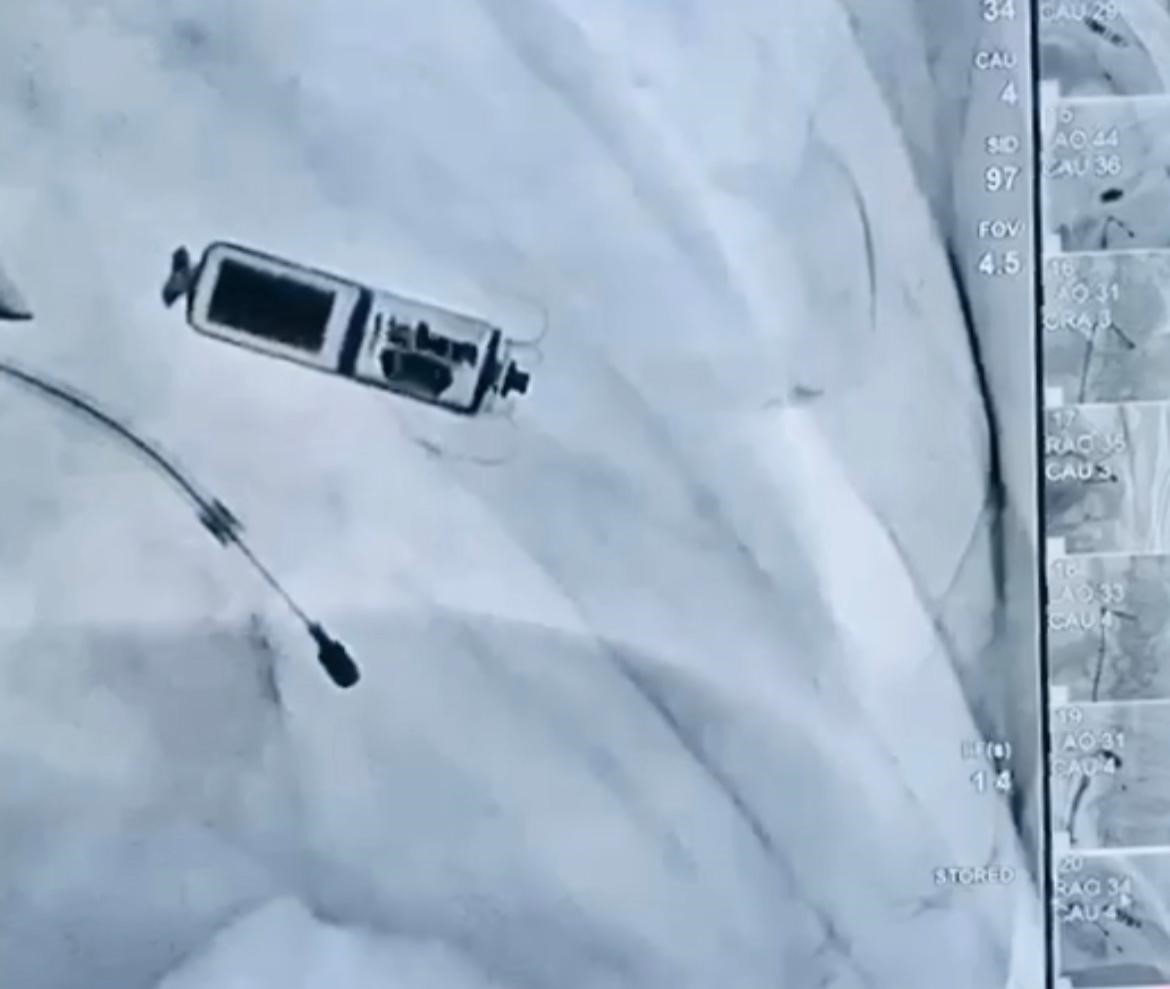
Leadless pacemakers have become a reality, thanks to the advances in battery technology, connectivity, and catheter-based delivery methods. Joining the league of advancements, on 18th December 2021, we performed the first case of AV Micra (Leadless Pacemaker) at Indraprastha Apollo Hospital, New Delhi which is the newest version of leadless pacing system.
Mr K (name changed because of confidentiality) 57-year-old male, developed symptomatic AV conduction disease. He was on dual antiplatelets drugs because of past history of angioplasty with drug eluting stents and anticoagulation because of paroxysmal atrial fibrillation. Hence, he accepted the option of a Leadless Pacemaker to avoid any complications related to transvenous implant procedure and pocket hematoma. He underwent a successful Micra (Leadless Pacemaker) implant and was discharged from the hospital within 24 hours.
This leadless device does not require cardiac wires (leads) or a surgical “pocket” under the skin to deliver pacing therapy. Less than one-tenth the size of traditional pacemaker, about the size of a large vitamin capsule, it can be implanted entirely inside the heart through a keyhole puncture in the groin. It is cosmetically invisible and is implanted directly into the heart -providing a safe alternative to conventional pacemakers.
Transcatheter Pacing System (TPS) uses self-expanding Nitinol tines to fixate in the trabeculae. Being invisible to the patient, it also helps them overcome the trauma of the surgery and helps them seamlessly return to their normal lifestyle.
Patients with prior device and lead infection, vascular access issues (dialysis, post-cath), Twiddler’s syndrome, renal failure, and tricuspid regurgitation have had success with leadless pacemaker. There are no lumps under the skin on the chest or leads anchored to the muscle bed while the leadless device is in place. Patients who have traditional pacemakers may experience slight discomfort as a result of them.
Historically, patients with AV block have been treated with traditional dual-chamber pacemakers, identical in size and shape to the original TPS. The latest advanced leadless pacemaker has several additional algorithms which detect cardiac movement, allowing the device to adjust pacing in the ventricle to coordinate with the atrium, providing “AV synchronous” pacing therapy to patients with AV block. More pacemaker patients qualify for a new treatment option that offers the advantages of leadless pacing.
With my 25 years of experience in the field of Cardiac Pacing and Arrhythmias, I have done maximum Leadless Pacemakers in the country. Having done the First Live Case of Leadless Pacemaker on 6th August 2016 at TCT, India, the first in Asia Pacific region, I have been doing the awareness, implantership, proctorship and training of the TPS all over the Asia Pacific region. The best of the wonders in the History of Pacing has been the Leadless Pacemaker technology.









Promoted by Fix Me Digitally