How the problems diagnosed?
To decide whether a pacemaker is needed, your doctor will ask about your symptoms and health history. You'll also have tests that check the speed and rhythm of your heartbeat. These include a painless test called an electrocardiogram (ECG). you may also be asked to wear a small electronic device, such as a Holter monitor or event recorder. These information about your heartbeat over a period of hours or days.
How can pacemaker help?
A pacemaker does exactly what its name says: It helps keep your heart beating at the right place. This reduces symptoms of a slow heartbeat. It can also let you take medications that would otherwise slow your heartbeat too much. Best of all, a pacemaker can improve your lifestyle by letting you be more active. Keep in mind, though, that having a pacemaker is a lifelong commitment. You'll need to see your doctor for regular checkups. You'll also need to take good care of your heart. But these things are more than worth it to keep your heart working well.
 (Source: https://www.americanewshour.com)
(Source: https://www.americanewshour.com)
Your heart's electrical system
Your heart is a muscle that pumps blood throughout the body. It does this using an electrical system that tells your heart when to contract (squeeze). If there's a problem with this electrical system, your heart may not beat as fast or as often as it should. This means that the heart can't pump as much blood as the body needs. When that happens, you can have symptoms such as lightheadedness as fatigue.
Signals tell the heart to beat
Each heartbeat starts with an electrical signal. The signals are sent and received by special electrical cells within the heart called nodes. As the signals move through the heart, they tell the chambers that pump blood (called atria and ventricles) when to contract. When you are active, the signals from the nodes speed up to pump blood faster. When you're resting, the signals return to a normal pace.
Problems with electrical signals
A slow heartbeat is often due to problems with the SA node or AV node. In some cases,the heartbeat is slow only once in a while. In others, the heart may beat slowly all the time. And sometimes the heart fails to raise the heart rate during increased physical activity. If either of the nodes fail to send a signal, the heart may go into an "escape rhythm". This means it continues to beat, but at a slower and less reliable pace.
Sick sinus syndrome
The main problem that affects the SA node is called sick sinus syndrome. It can cause any of the following:
- Sinus bradycardia occurs when the SA node sends out signals too slowly.
- Sinus pause occurs when the SA node fails to send a signal. Without a signal, the atria dont contract.
- Tachy-brady syndrome occurs when the SA node sends out signals that cause the heartbeat to alternate between very fast and too slow.
AV block ("Heart Block")
Heart block occurs when the AV node has problem passing on electrical signals to the ventricles. It can be caused by problems with either the AV node or the bundle branches. If the ventricles don't contract. This may happen only once in a while. Or, the signal may be blocked all the time.
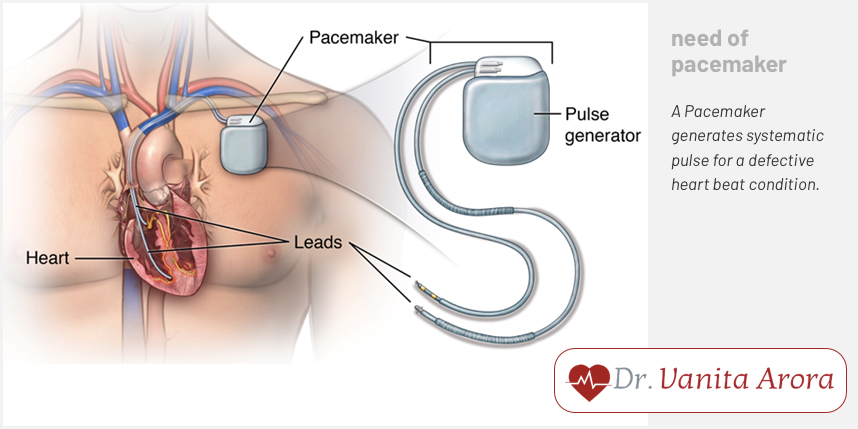
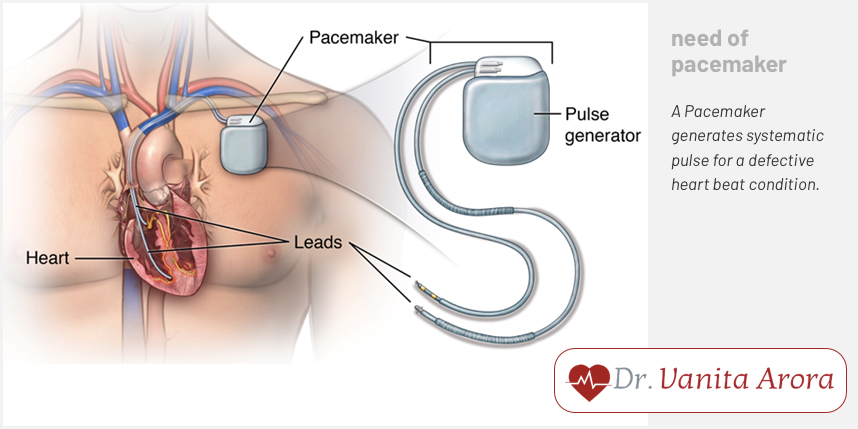
Understanding Pacemakers
A pacemaker is small, lightweight electronic device that helps correct a slow heartbeat. It does this using a tiny computer to send electrical signals to your heart. The signals tell the chambers in your heart when to contract. This keeps your heart beating at the right pace. Sensors in the pacemaker also keep track of your activity level and can adjust the signals as needed.
 (Source: https://www.philpoteducation.com/mod/book/tool/print/index.php?id=2871&chapterid=3025)
(Source: https://www.philpoteducation.com/mod/book/tool/print/index.php?id=2871&chapterid=3025)
The parts of pacemaker
Below are the three main parts:
- The connector or "healer" is the part of the generator where the lead (or leads) are attached.
- The generator sends out electrical signals. It has a smooth, lightweight case that contains a tiny computer and battery. It is placed in a "pocket" between your skin and chest muscle.
- Leads are wires covered by soft, flexible material. They are placed in a vein that goes to your heart. This lets them carry the generator's signals directly to the heart. Sensors on the leads also help the generator keep track of your heart's rhythm.
- Anchors on the tips of the leads attach the leads to the heart muscle.
Types of pacemakers
Your doctor will choose the type of pacemaker that's best suited for your condition. All pacemakers have the same basic design. The main difference is the number of leads that go to the heart. Most pacemakers have one or two leads. If you have a condition called advanced heart failure, you may be given a pacemaker with two or three leads (called a biventricular pacemaker).
A single-chamber pacemaker had one lead. The lead is usually attached to the right ventricle (the exact placement inside the ventricle may vary).
A dual-chamber pacemaker has two leads. One attaches to the right atrium. The other attaches to the right ventricle. Having two leads helps coordinate the signals that tell these chambers when to contract.
How a pacemaker adapts to your needs
When you're active, your heart beats at a faster pace to meet the body's need for more blood and oxygen. However, problems with the heart's electrical system can prevent the heart from speeding up. To fix this problem, all pacemakers have a rate-responsive feature. This means they can automatically adjust your heart rate as needed. The pacemaker speeds up when you're active, and returns to a normal pace when you're resting.
 (Source: https://www.verywellhealth.com/pacemaker-low-battery-replacement-1746230)
(Source: https://www.verywellhealth.com/pacemaker-low-battery-replacement-1746230)
The implantation procedure
Placing a pacemaker inside the body is called implantation. This is not the same as open heart surgery. Instead, it's a relatively minor procedure done in an operating room or cardiac catheterization lab. A pacemaker can be implanted in either side of the chest, but is most often placed on the left side. The procedure usually takes 1 to 2 hours.
Getting ready for your procedure
Follow all your doctor's instructions to prepare for the procedure. You may be asked to do the following:
- Tell your doctor in advance about any medications, supplements, or herbs you take. Also mention if you have any allergies to medications.
- Ask your doctor what to do if you take prescription blood thinners, such as Coumadin or Plavix. Stop taking aspirin, ibuprofen and naproxen if directed.
- Ask an adult family member or friend to give you a ride home after the procedure.
- Tell the doctor if you're left-handed or right-handed. Also mention if you often do activities that involve the chest and shoulder, such as shooting a rifle. These factors may influence which side of your chest the pacemaker is implanted in.
- Don't eat or drink anything after midnight, the night before your procedure. If you need to take medications, swallow them with just a small sip of water.
Before implantation
- On the day of the procedure, be sure to arrive at the hospital on time. Here's what to expect:
- You'll be asked to sign some forms and change into a patient gown.
- You'll be given an IV to provide fluids and medication. You may also be given medication to help relax.
- The skin where your pacemaker will be implanted is washed and may also be shaved.
During the procedure
The most common method for implanting a pacemaker is called endocardial ("inside the heart") implantation. This means that theleads run directly from the generator to the inside of your heart. In rare cases, the leads are attached to the outside of the heart. To implant the pacemaker:
- Medications are given to prevent pain. A local anesthetic is used to numb the site where the pacemaker is implanted. You may also br given medications to help you relax or sleep
- You'll be asked to sign some forms and change into a patient gown.
- You'll be given an IV to provide fluids and medication. You may also be given medication to help relax.
- The skin where your pacemaker will be implanted is washed and may also be shaved.
- An incision is made beneath your collarbone. A small "pocket" for the generator is then created. The incision also lets your doctor access a vein that leads to your heart.
- The leads are guided through a vein into your heart. An x-ray monitor helps your doctor guide the leads into place.
- The leads are attached to the heart using small anchors on the tips of the leads. Electrical measurements are done to find the best areas for placement.
- The generator is attached to the leads. Once the leads are secure, the generator is placed in the pocket beneath your skin.
- The incision is closed with sutures, surgical glue or staples. You'll then be taken to a recovery area.
Risks and complications
Although complications are rare, implantation does have certain risks:
- Bleeding
- Infection or nerve damage at the incision site.
- Severe bruising or swelling at the incision site.
- Puncture of the lung or heart muscle.
- Tearing of the vein or artery wall.
- Clotting or air bubbles in the vein.
- Heart attack, stroke, or death (very rare).
After the procedure
In most cases, you'll stay on the monitored bed overnight after your procedure. Before you go home, you'll receive discharge instructions. These tell you how to care for your incision. They also list precautions that will help protect your pacemaker as you heal. If you have any questions, be sure to talk with your doctor or the nurses.
In the hospital
After the procedure, nurses will monitor your heart signals and check your incision. They can also provide medications for pain. Be sure to tell the nurses if you have any chest pain, shortness of breath, twitching, or hiccups. Once you are stabe, you'll be moved to a hospital room. There your pacemaker's functions and settings may be checked. You'll also have a chest x-ray. You can go home once your doctor says it's okay.
Recovery at home
To help speed your recovery, be sure to follow all your doctor's instructions.
- You may be told not to raise your arm (on the side where the pacemaker is implanted) above shoulder level for a time. But don't stop using the arm or shoulder completely.
- You may have the bruising at the incision site for about a month. This is normal. It will go aya as the incision heals.
- You can often get back to your normal routine soon after implantation. Ask your doctor when you can return to work.
- You may be instructed not to drive for a certain amount of time. Your doctor will tell you more about this.
Caring for your incision
It's normal to have some pain and stiffness around your incision for a few days. over-the -counter pain medications can often help. If needed, your doctor may also prescribe pain medications. To care for the incision, use these tips:
- Change or remove the dressing as instructed by your doctor.
- Keep the incision clean and dry. You may be told to take sponge baths at first. You can begin showering when your doctor says it's okay.
- Don't scrub the incision as you bathe. Also, don't let water spray directly on the incision.
- Pat the incision dry. Don't use lotion, ointment, or powder on the incision while it heals.
- Call your doctor if you notice any changes in the incision, such as signs of infection.
When to call your doctor
Call your doctor if you have any of the following after your procedure:
- Signs of infection at the incision site, such as increasing redness, swelling, warmth or drainage.
- Fever over 100 F (37.7 *C)
- Pain around your pacemaker that gets worse, not better
- Chest pain or shortness of breath
- Bleeding or severe swelling of the incision site (bulging like a golf ball)
- Swelling in the arm or hands on the side of the incision site
- Twitching chest or abdominal muscles
- Frequent or constant hiccups
Checking your pacemaker
To ensure your pacemaker is working well, you'll need to visit your doctor or pacemaker clinic a few times each year. During these visits, the pacemaker's functioning and battery level are checked. If needed, your pacemaker's settings can also be adjusted. This helps fine tune the signals so the pacemaker is always doing its best or your heart.
Seeing your doctor
During pacemaker clinic visits, your doctor will check information that's stored on your pacemaker's computer. This is done by placing an electronic wand over the skin where the pacemaker is implanted. It will not cause any pain. The battery inside the pacemaker is also checked. If the battery begins to run low, the pacemaker sends out a signal that can be seen during these tests. And if the battery is low, your doctor will schedule a time to replace it. In the meantime, your pacemaker will still continue to work normally.
How long will my pacemaker last?
Pacemakers are very reliable. The batteries usually last around 10 years. In rare cases, the leads may also wear out and need to be replaced.
Replacing the battery
Your pacemaker is sealed inside the generator. So replacing the battery also means replacing the entire generator. This is done with a procedure that is simpler and shorter than the initial implantation. Once the old generator is removed, the new generator will be placed in the same 'pocket' in your chest. You can go home the same day.
 (Source: https://economictimes.indiatimes.com/magazines/panache/light-is-power-new-pacemakers-con-stimulate-heart-muscle-in-a-unique-way/articleshow/67075592.cms)
(Source: https://economictimes.indiatimes.com/magazines/panache/light-is-power-new-pacemakers-con-stimulate-heart-muscle-in-a-unique-way/articleshow/67075592.cms)
Replacing the leads
To replace leads, you'll have a procedure that is very similar to the one used to implant the pacemaker. In some cases, though, the new leads may need to be placed in a different vein on the opposite side of the chest. This means that the generator will also have to be moved to the opposite side of the chest.
Living with a pacemaker
Living with the pacemaker isn't hard. Its safe for you to do almost any activity you like. There are few things, though, that you'll need to keep in mind. These include being aware of electronic signals that could interfere with your pacemaker. You'll also need to carry a pacemaker ID card. And to keep your heart in good shape, be sure to get regular exercise and see your doctor for checkups.
Your pacemaker and outside signals
Most machines and devices will NOT interfere with your pacemaker. For example, it's safe safe to use microwave ovens, computers, radios, and televisions. Hair dryers, electric blankets and most power tools are also okay. However, you will need to use caution around certain devices. If you are not sure whether a device is safe, ask your doctor or call the pacemaker manufacturer.
Signals that can cause problems
A few things can create signals that may interfere with your pacemaker. In general, these signals wont permanently damage your device- or harm your heart. You should contact your doctor, though, if any of the following cause symptoms:
- Cellular phones should be kept 6 inches away from your generator. As you talk, hold the cell phone to the ear on the opposite side of your pacemaker. Carry the phone on the opposite side as well.
- Electromagnetic anti-theft systems are often located near store entrances and exits. Walking through one is okay. But avoid standing or leaning against one.
- Very strong magnets should be avoided.never have an MRI test. You should also avoid standing near large speakers, such as those used for music concerts.
- Strong electrical fields can be created by radio towers and heavy duty power equipment (such as arc welder). Car engines also create an electrical field while they are running. So avoid leaning over the hood of a running car.
Carry ID card
You will receive an ID card that contains important information about your pacemaker. Show the ID card to any healthcare provider you visit. You may also need to show the card to security staff at times. This is because pacemakers tend to set off the security devices found in the stores and libraries. likewise , be sure to show your card to the security guards at the airport. This lets them know to follow special procedures that prevent the security wand from interfering with your pacemaker.
Exercise regularly
Having a pacemaker doesn't mean you can't be active. In fact, you may find that exercising is even easier with a pacemaker. For best results, try to be active at least 30 minutes each day. Most activities are fine. But talk with your doctor if you play contact sports or do weightlifting. In some cases, these could damage your pacemaker. And if you are not sure where to begin, ask your doctor for advice. He or she can help design an exercise program that fits your needs.
Keep seeing your doctor
To get the best results from your pacemaker, keep seeing your doctor for regular checkups. These let your doctor review your heart's electrical activity. They also make sure the pacemaker is doing all it can fro your heart. And if you have any symptoms that concern you, be sure to give your doctor a call.
Feeling good again
A pacemaker is a small device, but it can make a big improvement in how you feel. By keeping your heartbeat at the right pace, a pacemaker can allow you to be more active. It can also help you feel more confident about your heart and your health. This makes it easier to focus on the things in life that mean the most to you.
 (Source: https://www.americanewshour.com)
(Source: https://www.americanewshour.com)
 (Source: https://www.philpoteducation.com/mod/book/tool/print/index.php?id=2871&chapterid=3025)
(Source: https://www.philpoteducation.com/mod/book/tool/print/index.php?id=2871&chapterid=3025)
 (Source: https://www.verywellhealth.com/pacemaker-low-battery-replacement-1746230)
(Source: https://www.verywellhealth.com/pacemaker-low-battery-replacement-1746230)
 (Source: https://economictimes.indiatimes.com/magazines/panache/light-is-power-new-pacemakers-con-stimulate-heart-muscle-in-a-unique-way/articleshow/67075592.cms)
(Source: https://economictimes.indiatimes.com/magazines/panache/light-is-power-new-pacemakers-con-stimulate-heart-muscle-in-a-unique-way/articleshow/67075592.cms)